Xanax is a popular anti-anxiety medication that can be addictive if misused. What exactly is Xanax, and how does it work? Xanax, a brand name for alprazolam, is a benzodiazepine. It acts on your central nervous system, calming and relieving anxiety and panic.
Xanax works by slowing activity in your brain to promote relaxation and ease anxious feelings. It targets gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits excessive activity in your nervous system. By boosting the effects of GABA, Xanax helps calm your mind and body.
While effective when used as prescribed, Xanax also has a high potential for addiction and dependence. The sedative effects can be pleasant and lead to cravings for the drug. Misuse or high doses of Xanax, especially when combined with other substances, pose serious risks.
If you’ve been taking Xanax for an extended time or in high amounts, detoxing from it requires medical supervision. Abruptly stopping the drug can lead to withdrawal symptoms, so tapering off under the guidance of a doctor is critical.
Understanding Xanax Addiction and Dependence
If you’ve been taking Xanax regularly, your body has likely developed a dependence on it. This means that stopping abruptly can lead to withdrawal symptoms. The severity depends on factors like how long you’ve been taking Xanax and the dosage. The best way to detox from Xanax is under medical supervision. A doctor can develop a tapering schedule to reduce your dosage slowly over time. This helps minimize withdrawal effects. They may switch you to a longer-acting benzodiazepine during the process. Medications or therapy may also be used to manage specific symptoms.
Xanax Detox
The detox process from Xanax is challenging but necessary to overcome your dependence. As with any benzodiazepine, Xanax should not be stopped abruptly. Tapering your dosage under medical guidance is the safest way to detox.
Seek help from an addiction specialist to develop a customized tapering schedule. They can prescribe longer-acting benzos or other medications to minimize withdrawal symptoms as you slowly reduce your Xanax dose. Inpatient or outpatient treatment programs offer round-the-clock medical support in case of emergencies during detox.
Detoxing from Xanax at home is dangerous and not recommended. However, if done under medical guidance, a slow taper using a longer-acting benzo can be successful for some. The key is to go slowly, listen to your doctor, and ask for help immediately if withdrawal symptoms become severe.
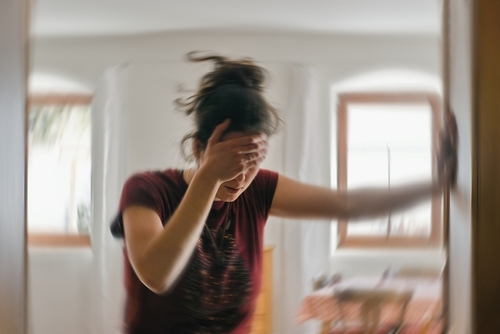
Rebound anxiety and insomnia are common during Xanax detox. Other potential side effects include nausea, vomiting, tremors, and seizures in severe cases. The good news is these symptoms are temporary, even though the process can be difficult.
Read more: Does Your Body Detox From Drugs When You Start Eating Healthy?
Can You Quit Xanax Cold Turkey?
No, quitting Xanax cold turkey is extremely dangerous and not recommended. Because of the severe withdrawal symptoms, medical detox is the safest way to stop using Xanax.
Quitting Xanax abruptly can lead to life-threatening side effects like grand mal seizures, where your brain loses control of normal functions like breathing. Even a short seizure can cause permanent damage or death without emergency care.
The psychological withdrawal symptoms from quitting cold turkey can also be dangerous. The extreme discomfort may drive you to use Xanax or other substances again to relieve the symptoms.
The only safe way to detox from Xanax is under medical supervision. Doctors can prescribe medications and taper your dose over time to minimize withdrawal symptoms. They also monitor you for dangerous side effects 24/7 and can provide emergency care.
How Much Xanax Causes Withdrawal?
If you’ve been taking Xanax regularly for an extended period, especially in higher doses, you’re at risk of developing a dependence on the medication and experiencing withdrawal symptoms when you stop taking it.
Even relatively small doses of Xanax, around 0.5 to 2 mg per day, taken consistently for 6-12 weeks, can lead to withdrawal for some people when discontinued. Higher doses of 3-4 mg daily make severe withdrawal symptoms more likely. While lower doses may reduce risks, there is still a chance of becoming dependent on and experiencing withdrawal from Xanax.
The longer you take Xanax and the higher the dose, the greater the chances of withdrawal. If you’ve been on Xanax daily for months or years, withdrawal should be done under medical supervision. A doctor can help create a customized tapering schedule to minimize withdrawal severity.
Xanax Withdrawal Timeline
The withdrawal from Xanax is intense, but the good news is the worst will be over within two weeks.
6 – 12 hours: The effects of your last Xanax dose are wearing off, and withdrawal symptoms start to kick in. You’ll feel anxious, irritable, and on edge. These feelings will intensify over the next few days.
Days 1 – 4: This is when withdrawal hits hardest. Rebound anxiety and sleep problems are at their worst. You may experience shaking, muscle aches, and sweating. The symptoms during this period can be difficult to deal with, so get support from loved ones or talk to a doctor about medication or therapy options to help ease this stage.
Days 7 – 14: The most severe symptoms have passed, but anxiety, insomnia, and discomfort can persist. While the symptoms are becoming less intense, protracted withdrawal symptoms may appear suddenly. Stay patient and continue self-care.
Days 15+: Most physical symptoms will have subsided, though psychological effects may linger. Practice relaxation techniques like meditation or yoga to help restore your mind and body to balance. Connecting with others who have gone through similar experiences can help provide motivation and accountability.
Xanax Withdrawal Symptoms
As your body detoxes from Xanax, you can expect to experience uncomfortable physical withdrawal symptoms. Some of the most common ones include:
Anxiety. Feeling on edge, restless, and worried.
Sleep problems. Difficulty falling or staying asleep, insomnia.
Sweating. Excessive perspiration and cold sweats.
Loss of appetite. Lack of interest in food or eating.
Muscle spasms or tremors. Uncontrollable jerking movements or shaking.
Hypersensitivity. Heightened sensitivity to light, sounds, touch, or smells.
Stomach issues. Nausea, vomiting, diarrhea or cramps.
These symptoms are most severe during the initial detox period, typically lasting 7 to 10 days after stopping Xanax. Staying hydrated, eating healthy, and exercising can help relieve discomfort. See a doctor for medication or treatment if symptoms become unbearable or last over two weeks.
Read more: Overcoming Fear And Anxiety In Detoxification
Contributing Factors That Affect Xanax Withdrawal
Several factors can influence the severity and duration of Xanax withdrawal.
Metabolism: As you get older, your body may metabolize Xanax more slowly. The same is true if you have liver disease or are obese. This means the drug can stay in your system longer, potentially worsening withdrawal effects.
Dosage and Duration: Higher doses, longer usage periods, and combining multiple benzodiazepines can intensify withdrawal. Xanax is a short-acting benzo, so stopping after long-term use or high doses can trigger severe rebound anxiety and other symptoms.
Individual Differences: Each person’s withdrawal experience is unique. Underlying health issues, genetics, environment, and psychological factors affect how your body responds to Xanax detox. Some people report few problems, while others struggle with protracted withdrawal lasting weeks or months. A strong support system will help you cope during this difficult process.

What Medication Is Used to Treat Xanax Withdrawal Symptoms
To ease Xanax withdrawal symptoms, several medications may be used. Doctors often prescribe longer-acting benzodiazepines like chlordiazepoxide or clonazepam. These are gradually reduced over time. Studies show anticonvulsants, antidepressants, and beta blockers can also help alleviate symptoms.
Doctors may switch you to a longer-acting benzo, then slowly decrease the dosage. Chlordiazepoxide or clonazepam are common. These have a longer half-life, so withdrawal happens more gradually.
Flumazenil can block Xanax’s effects at receptors, relieving acute symptoms. Anticonvulsants like gabapentin reduce seizures and anxiety. Antidepressants, especially SSRIs and SNRIs, boost mood and ease irritability. Beta-blockers reduce physical symptoms like increased heart rate.
What is Xanax Post-Acute Withdrawal Syndrome?
After stopping Xanax, the leftover effects in your body and brain can last for weeks or months. This is known as post-acute withdrawal syndrome or PAWS. During PAWS, you may experience anxiety, insomnia, cravings, and mood swings that come and go.
As your brain chemistry stabilizes, the symptoms will gradually decrease in frequency and intensity over time. Stay patient and focus on self-care. Connecting with others in recovery, eating healthy, exercising, and practicing mindfulness can help ease symptoms.
If PAWS symptoms become severe or last over a few months, talk to your doctor about treatment options, such as therapy or medication to manage specific symptoms. Remember, PAWS will pass. Stay committed to your recovery and know that sobriety and health are worth the fight.
At-Home Detox vs. Inpatient Detox
Detoxing at home can be difficult and potentially dangerous, especially from a benzodiazepine like Xanax. While inpatient treatment provides 24/7 medical supervision and support, detoxing at home may be an option if you have a strong support system and take proper precautions.
If detoxing at home, have friends or family stay with you around the clock for at least the first week. Taper slowly by cutting your dose by no more than 0.5 mg every 1-2 weeks. This gradual reduction will minimize withdrawal effects.
However, if symptoms become unbearable, seek medical help immediately. Stock up on over-the-counter medications for symptoms, like Imodium for diarrhea, ibuprofen for body aches, and melatonin for sleep. Stay hydrated and try to eat healthy, balanced meals.
The decision to detox at home or in a facility depends on your dosage amount, length of use, withdrawal severity, and available support level.
Managing Xanax Withdrawal Symptoms and Cravings
Managing the withdrawal symptoms from Xanax can be challenging, but there are some effective strategies to help cope during this difficult process.
Practicing relaxation techniques like meditation, yoga, or deep breathing can help ease anxiety and stress. These techniques activate your body’s relaxation response, slowing your breathing and heart rate. Taking short breaks to do light exercises like walking or stretching may relieve withdrawal symptoms.
Staying active and exercising regularly also releases endorphins that improve your mood. While the cravings and discomfort may seem unbearable, remember that this will pass. Celebrate each small win and milestone along your journey to overcoming addiction. You should feel proud of your progress and stay motivated to continue progressing.
With the support of your doctor and counselor, utilize the resources available to help you succeed. Don’t lose hope – freedom from addiction is possible and within your reach. Stay focused on your goal and keep putting one foot before the other. You’ve got this!
Contact MD Home Detox
Once you’ve made the important decision to detox from Xanax, the next step is to get the help and support you need. Call MD Home Detox and one of our admissions agents can help you choose one of our at home detox programs. Our doctors, nurses, and detox specialists will come to your home and help you detox from Xanax without uncomfortable withdrawal symptoms.


